Long Term Care COVID-19 Situation Report
Thursday, December 3, 2020
(0 Comments)
Posted by: Alyse Meyer
Long Term Care COVID-19 Situation Report
The Growing Threat of Coronavirus in Texas Communities
Texas currently has the second highest number of confirmed COVID-19 cases in the United States. The state currently ranks 2nd in the nation for the number of deaths surpassing 21,000 this month.
- 1,157,000+ cases
- 40.32 cases per 1,000 people statewide
- Statewide positivity rate surpassed 10% in late October
- 21,000+ deaths
Threat to Texas’ Older Population
- There are an estimated 3.5 million people in Texas age 65 and older; they make up approximately 12.3 percent of the total Texas population of 28.7 million.
- 80% of all US COVID-19 deaths are among people 65+—a death rate at least 90 times higher than 18-29 year-olds.
About 1% of the U.S. population live in nursing homes and other long-term care settings, but represent 40% of COVID-19 deaths, according to the COVID Tracking Project.
- DSHS reports Texans 65+ account for approximately 10% of all reported cases, but over 70% of all reported deaths.
- Nursing homes with higher numbers of Black or Hispanic residents have been disproportionately affected by COVID-19, as measured by the share of nursing homes reporting deaths, share reporting cases, and the severity of outbreak.
- Rates of depression and anxiety are high among adults ages 65 and older relative to 2018 rates,
with one in 4 reporting anxiety or depression during most weeks since the pandemic’s start.
- In 2019, over 90,000 Texans resided in nursing homes. Texas HHSC reported over 2,000 assisted living communities representing approximately 75,000 beds. Thousands more live in independent retirement communities and affordable senior housing.
Enhanced Infection Control Measures to Prevent & Mitigate COVID-19
- Nursing homes implemented enhanced infection control procedures, routine screening of all entrants and staff, and use of personal protective equipment by all residents and staff.
- CMS issued guidance on the restriction of nonessential medical staff and all visitors except in certain limited situations, and additional measures on March
13, 2020. Governor Abbott extended visitation restrictions to all long-term care facilities in Texas.
- CDC issued guidance specific to nursing homes and long-term care facilities.
- CMS issued a call to action for nursing homes and state and local governments reinforcing
infection control responsibilities and encouraged agencies to work closely with nursing homes on access to testing and PPE.
- Focused Infection Control Surveys are conducted and enhanced enforcement action is taken based on COVID-19 data and inspection results.
- Texas HHSC issued COVID-19 Response Plan for Nursing Facilities and Assisted Living.
- Governor Abbott directed HHSC to conduct baseline testing on all nursing home residents and staff in May 2020.
- Special Infection Control Assessment (SICA) conducted on-site assessments at nursing facilities to identify infection control concerns and provide immediate recommendations and guidance to facility leadership on infection control practices and mitigation
strategies.
- CMS mandated routine COVID-19 testing of nursing home staff in August 2020.
- HHS deployed point-of-care testing devices to certified nursing facilities to assist with ongoing testing requirements.
Testing Needs Among Older Adults & Care Providers
- Aging services providers need ongoing access to accurate rapid-results testing, including antigen and PCR tests, delivered as part of a national or state testing strategy, as well as the resources to pay for tests and ongoing testing.
- Providers report using a mix of testing types, including PCR tests with collections taken onsite and sent to an outside lab, and point-of-care antigen tests.
- The federal government has not yet provided adequate levels of desperately needed resources to enable the regular, ongoing testing of older adults and care workers in all aging services settings. Texas may support mandated ongoing testing by allocating
state testing supply resources.
- Nursing homes are required to outbreak test and routinely test staff either monthly, weekly or twice a week depending on county positivity rates.
- Providers working in care settings that must meet testing mandates are sometimes forced to navigate multiple mandates on testing—federal, state, and local—which can result in confusion and duplicative efforts.
Federal & State Testing Resources
The Trump Administration has provided some patchwork testing resources to some aging services providers, including nursing homes, assisted living and hospice. There is still no coordinated national testing strategy for aging services, which would
address all settings and staff. Texas has provided some testing support to providers but access to these resources has been extremely limited throughout the pandemic.
- BD or Quidel antigen testing machines have been sent to 14,000 certified nursing homes in the US. Only 1-2 weeks of testing supplies were sent for use with the delivered antigen machines. The majority of machines sent, by BD, have a limited life
expectancy of 3,000 tests or maximum of 34 months from date of manufacture.
- 150 million Abbott BinaxNOW one-time use tests are being distributed by HHS; 49 million are designated for aging services providers, including home health and hospice agencies, nursing homes and assisted living.
- Nursing homes will get 18 million of these. For a nursing home with 300 staff that test twice a week, their allotment would only last 1-2 weeks.
- Assisted living providers will get 15 million.
- Texas was allocated a supply of Abbott BinaxNOW tests and has the ability to distribute an additional supply to long-term care facilities. Currently, those tests have only been allocated to support essential caregiver testing.
Other settings where older adults live, like affordable senior housing, independent living communities, and community-based services, have been relatively ignored.
Testing Costs
Aging services providers must locate and pay for much of their testing-related resources and activities, including test supplies, shipping PCR test samples to labs, and hiring or training staff to perform the tests, as well as the PPE that must
be used while administering the tests. With no end to the pandemic in sight, these costs—for tests alone—are unsustainable.
- PCR tests, which are the only option for many providers, cost $100-$200.
- A one-time PCR test for every staff and resident in nursing homes and assisted living in the US alone would cost $672 million.
- Antigen test kits from BD or Quidel, which cost $20-25 each, must be purchased from the manufacturer (resupplies were not available for weeks, though the companies say they are available now).
- Expenses for antigen testing in a 150-bed nursing home can range from $3,750-$15,000 per week, depending on staffing levels and community COVID-19 positivity rates.
- Additional supplies of Abbott BinaxNOW tests will have to be purchased for $5/test from the manufacturer, although inventory is not currently available (HHS is controlling distribution).
Personal Protective Equipment (PPE) Shortages & Costs
Aging services providers need ongoing, reliable access to large quantities of PPE to stop COVID-19 from spreading. Texas must make these facilities a top priority when emergency PPE requests are made.
- Aging services providers have been left largely on their own to acquire all types of PPE, including gloves, gowns, masks, eye protection, etc.
- Aging services providers are using an amount of PPE that is astronomically higher than before the pandemic.
- Some PPE supply has improved, but providers are still facing significantly higher than normal prices, creating significant financial pressures. One Texas community reported paying $7.00 per gown compared to .60 cents normally.
- Some aging services providers say they are spending a year’s worth of their PPE budget in one month alone. This is not
sustainable.
- A leading supplier estimates PPE products are now 4-8 times more expensive than before COVID-19, especially gowns and
masks.
- Across the country there have been rolling shortages of various types of PPE (the FDA began creating lists of shortages) that escalate prices. “There’s very much a ‘Groundhog Day’ feel to all of this,’ says Professor David Grabowski.
Staffing Shortages Among Aging Services Providers
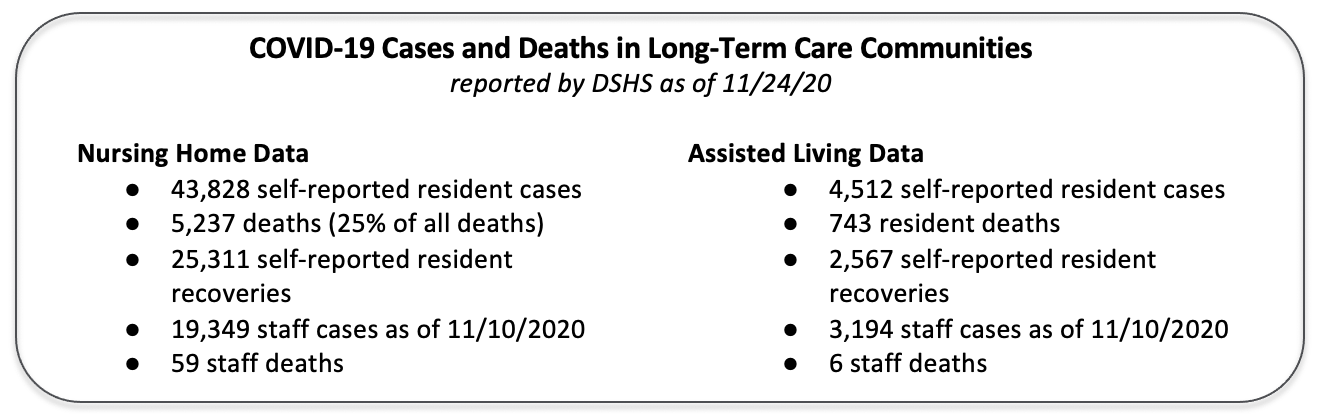
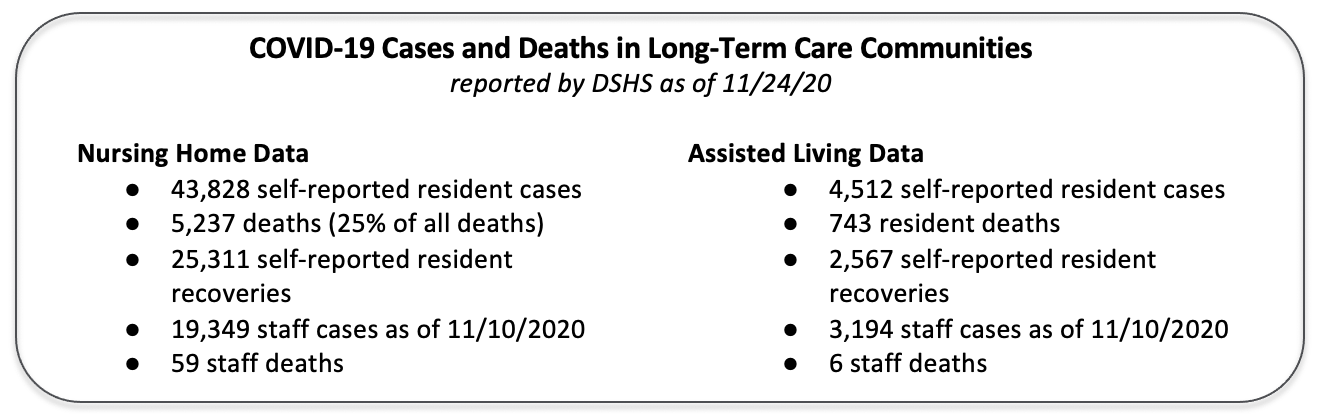
- Over 22,000 nursing home and assisted living staff have contracted COVID-19. 65 have died.
- Continued growth in positive cases among staff threaten staffing levels and service delivery, and drive additional costs for overtime and staff replacement.
- Provider requests to the state for emergency staffing are increasing, as well as use of staffing agencies to fill current vacancies. Some providers have reported paying double the average hourly wage of RNs, LVNs, and CNAs to hire through
staffing agencies.
- Dedicating staff to resident cohorts and COVID-19 isolation units to care for infected residents further depletes available and already overburdened staff.
- On October 19, 2020 US Department of Health & Human Services released COVID-19 Intensifies Nursing Home Workforce Challenges.
The report makes recommendations to federal and state governments to maintain adequate staffing levels and quality resident care.
State Actions to Support Provider Mitigation Efforts
Financial Strain Among Aging Services Providers
Aging services providers continue to face exponential expenses from testing, PPE, staffing, cleaning and other ongoing costs, while revenues have fallen substantially for many.
- Nursing homes and assisted living across the country are reporting operating losses of several hundred
thousand dollars a month or more, and many affordable senior housing providers have COVID-related expenses far beyond their means.
- In nursing homes, short-stay/rehab admissions are falling as the volume of surgeries and medical care has declined and hospitals discharge patients to home care settings. At the same time, long-term care admissions have fallen as families
have stopped bringing their older relatives to nursing homes.
- The pandemic has triggered revenue losses of up to 23% in nursing homes, and nursing homes have
begun to close.
- Almost ¾ of nursing homes (72%) reported they will be unable to maintain operations for another year at
this rate—and 40% said they would last less than six months.
- Not all long-term care providers have had access to federal funding relief including private-pay nursing facilities and assisted living communities.
- A Texas continuing care retirement community reported, on an annualized basis, approximately $2,900,000 in incremental costs as a result of the COVID-19 pandemic. These costs will continue for the foreseeable future with not relief
in sight. In addition to these incremental costs, the community has suffered a loss of revenues on an annualized basis of approximately $9,000,000.
- Home health, hospice, PACE organizations, and residential settings like assisted living have also faced significant new financial pressure. PACE organizations are ineligible for federal dollars despite providing critical health and
long-term care to their participants.
|